Abstract
Introduction: Iron is essential for the function of many key proteins including hemoglobin (Hgb) and myoglobin (involved in oxygen transport/exchange), cytochromes (involved in energy generation), various enzymes (involved in cell proliferation and neurotransmission), and immune function. Iron deficiency can, therefore, negatively impact patients' health-related quality of life (HRQOL) and requires treatment to replete iron stores. Although oral iron is a common initial treatment, some patients do not tolerate it or fail to adequately respond, and many of these patients live with chronic anemia and the related negative effects on their HRQOL. A Phase 3 double-blind, placebo-controlled trial (NCT01114139) had previously found that patients with iron deficiency anemia (IDA), unsuccessfully treated with oral iron, had very poor baseline HRQOL scores associated with fatigue, and that IV iron treatment with ferumoxytol resulted in clinically meaningful improvements, significantly greater than placebo, over the 5-week study period. To explore the durability of this treatment effect, this analysis reports on the impact on patient-reported outcomes (PRO) of a single course of ferumoxytol therapy over the course of the subsequent 6-month extension study.
Methods: A 6-month Phase 3, open-label extension study (NCT01114217) was conducted in patients who had completed the double-blind, placebo-controlled Phase 3 trial. Enrolled patients were evaluated for IDA monthly throughout the study period. Those with persistent or recurrent IDA (Hgb <11.0 g/dL and TSAT <20%) at any evaluation visit, received a course of ferumoxytol (2 x 510 mg, 3-8 days apart). The same validated PRO instruments were administered in this extension study as in the preceding double-blind trial: Functional Assessment of Chronic Illness Therapy-Fatigue Scale (FACIT-Fatigue), Short Form Health Survey (SF-36), and Linear Analogue Scale Assessment (LASA) of Energy, Activities of Daily Living (ADL) and HRQOL. This analysis reports results for the subgroup of patients who did not receive any additional doses of ferumoxytol during the entire 6-month period of the extension study.
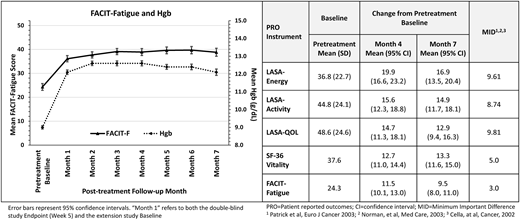
Results: The majority of patients enrolled in the extension study who had received ferumoxytol in the previous Phase 3 trial (285/471; 61%) did not meet the above-noted re-treatment criteria during the 6-month extension, and did not receive any further doses of ferumoxytol. Reflecting the overall enrollment in the extension study, these patients were predominantly female (90.0%) and white (63.5%), with mean age of 43.6±13.3 years (range 19-88). The most common primary underlying conditions were abnormal uterine bleeding (41.8%), GI disorder (33.0%), and cancer (10%). Their mean Hgb had increased from 9.0±0.8 g/dL at Baseline to 12.1±1.1 at Week 5 of the double-blind trial and remained above 12.0 throughout the 6-month extension study visits (Month 7 Hgb 12.1±1.2) despite receiving no further ferumoxytol.
At Baseline of the double-blind trial, their FACIT-Fatigue scores were lower (24.3±12.3) than general (non-anemic) US population norms (40.1-43.6), and comparable to anemic cancer patients receiving chemotherapy (23.9, Cella 2002). By Week 5 following ferumoxytol treatment, their FACIT-Fatigue scores had increased significantly (36.1±11.2), approaching general population norms. This improvement was sustained over the following 6 months (Month 7 score 38.8±11.5).
Their SF-36 Vitality scores increased from 37.6 ±11.8 at Baseline of the double-blind trial to 47.7±12.0 at Week 5, approaching the general US population norm (50.0, McHorney 1993) and continued to increase slightly over the next 6 months (Month 4, 50.0±12.0; Month 7, 50.9±11.5). Similarly, the significant improvements in LASA Energy, ADL and HRQOL scores that were observed in the double-blind study were also maintained over the next 6 months.
Conclusions:These data suggest that ferumoxytol may provide important clinical benefits to IDA patients with a history of unsatisfactory oral iron therapy; these benefits include reductions in fatigue, increased energy, vitality, and ability to perform ADL and improved HRQOL. This is important especially in light of the poor baseline energy and HRQOL scores of patients who cannot take oral iron. This study found that for the majority of patients, these improvements were sustained for at least 6 months after a single course of therapy.
Vadhan-Raj:AMAG Pharmaceuticals, Inc: Other: received funding from Amag to support clinical trial. Dahl:AMAG Pharmaceuticals, Inc: Employment, Equity Ownership. Jiang:AMAG Pharmaceuticals, Inc: Employment, Equity Ownership. Strauss:AMAG Pharmaceuticals, Inc: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.